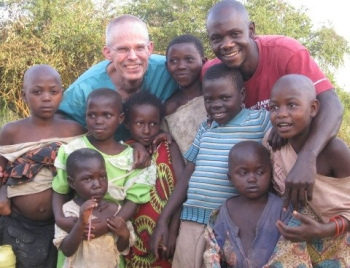
© 2009 Medical Teams International. Photos courtesy of Randy Jacobs / MTI
MTI Press Release: January 5, 2009
This Wednesday, January 7th, a volunteer doctor from Bend, Oregon, working with Medical Teams International, departs to care for families fleeing the rebel fighting in the Democratic Republic of Congo.
Dr. Randall (Randy) Jacobs will work in a Ugandan refugee camp, where thousands of Congolese people are seeking medical care, food, clean water, and shelter. Dr. Jacobs, a physician at Bend Memorial Clinic, will serve a month-long assignment in Juru, Uganda. He joins Colleen Bradley, a volunteer nurse from Montana, and additional staff from the agency’s Ugandan office.
Aid workers estimate that more than 5.4 million people have died in this decade-long conflict, which primarily affects the central African countries of Rwanda, the Democratic Republic of Congo, Sudan and Uganda. Up to 45,000 people continue to die each month — most of them women and children — from easily treated diseases like malaria, upper respiratory conditions and chronic diarrhea. These diseases run rampant in the camp environment, where sanitation and hygiene are marginal.

“The situation in the Congo is heartbreaking,” says Joe DiCarlo, director of emergency relief at Medical Teams International. “Entire villages are burned. Children kidnapped; the women raped. Even if families survive the rebel attacks, they face additional hardships and health challenges due to the lack of medicines, adequate shelter and basic necessities.”
Dr. Jacobs and nurse Bradley will carry in nearly $15,000 in antibiotics, bandages, and anti-malarial medication when they arrive. This past December, Medical Teams International sent more than $560,000 in medical supplies to help families affected by the Congo conflict.
Dr. Jacobs is due to return February 6th.
Excerpts from Dr. Jacobs’ Diary: January 16
We saw 125 patients today. Many had severe malaria, dysentery and dehydration requiring IV fluids and antibiotics. One baby arrived with severe malaria….
My translater, Jerome, discussed his current situation with me today. His family escaped the Congo, where he worked as a tour guide in a national park. I am sure he was pretty well off there, but now he, his wife and their three children are living under a tarp. We did our best to encourage him, but it is a difficult situation.
Our director had a positive meeting with UNHCR today. They are very impressed with our services and asked Medical Teams International to submit a grant proposal for additional clinical services, including nutrition, HIV testing and counseling, and immunizations. It appears that we’ll continue to work here long-term. We also learned that Medical Teams International will send another volunteer medical team from the U.S. I am so thankful and so are the Ugandan staff.
January 17

A 46-year-old refugee arrived from Kabahinda transfer center with his family today. His blood sugar was more than 500, but he refused a hospital transfer because his family is living in the bush without shelter. We have no diabetes medicine here, so he needs to head to the hospital. Hopefully, he will survive the weekend and return Monday for a hospital transfer. We continue to treat severe malaria and pneumonia. One patient arrived with a fractured hand, and a splint worked great. We are all now known as the Medical Teams International Power Rangers — fighting disease.
January 21
… We’re able to refer a four-year-old with mental retardation and probable cerebral palsy. A social worker came to camp to assess the child. We saw more pneumonia, malaria, PID, HIV, probable TB, dysentery, wounds, skin infections and pregnancies.
We treated about 120 people and returned home by 7 pm…. May your day be blessed!
January 22
Heavy rain fell all morning and the roads continue to be a challenge. The rains prevented many patients from coming this morning, but we made up for lost time with a busy afternoon. The weather cleared and we were able to treat 120 patients after lunch.

We met an infectious disease and international health physician from Harvard who travels here for a week every month to coordinate HIV training programs for Harvard and MIT students. Good debriefing on services. The regional referral hospital here does not have functioning X-ray or ultrasound, and he has found very poor quality in lab. Nearest CT and MRI machines are in the capital, but are only available if the patient can pay cash. I can’t imagine trying to care for the complex referrals with such limited diagnostic equipment. So it is here….
January 23
Clear, warm day today. We saw 165 patients, plus 35 antenatally. A three-year-old arrived with weight loss and is probably HIV positive. We offered an HIV test to both mother and child, but the mother refused and left the clinic.

An eight-year-old Congolese refugee arrived with extensive burns. The rebel troops killed his father and then poured boiling water on him. Part of his ring finger was badly damaged from a bore hole pump. We were able to shorten his finger and close the wound. He was so incredibly brave and did not complain for a moment. He expressed his thanks in French as he left. He was an amazing child. We trained the staff while we repaired his finger.
We’ve seen several cases of severe malaria in both children and adults. On the way back from the field, we passed an abandoned car. It is common to see broken cars simply left in the middle of the road. On its back window, someone had placed vinyl letters reading, “No situation is permanent.” Their car must have broken down before!
January 24
Doing well and loving the work, which continues to be busy. The refugee population finds that we offer dependability, quality and expanding services. The staff were sad last night when they realized we depart in two weeks. Fortunately, a new team is arriving to carry on the work.
January 28

We had a warm and dry day. My hand-laundered clothing is finally drying out. We had 165 patients today. Another U.S. nonprofit is building a nursery school adjacent to our site, complete with climbing sets for the kids.
Our lead interpreter, Ibrahaim, is amazing. He’s 25 and speaks seven or eight languages, including French, English, Kiswahili and Congolese tribal dialects. He is a strong leader and a hard worker. He doesn’t share much about his personal history but he left Congo about six months ago after being a military leader. He is respected by all the refugees here and is trying to support extended family on his wage of $3 per day.
January 29

This was an exhilarating and exhausting day. It began with a deep hand abscess, which required extensive cleaning, packing and draining.
Then a three-year-old arrived with her entire right arm swollen to twice its normal size. A six-foot Black Mamba snake crawled into her family’s tarp shelter and bit her arm during the night. These snakes are the largest venomous snakes in Africa and are the second largest in the world. They can strike up to 12 times and inject a lethal venom each time. Death usually ensues within two to three hours, but God is obviously protecting this child. She was bitten eight hours before arriving at our clinic and showed no signs of shock, hemorrhage or convulsions. We provided emergency care, removed the tourniquet and transfered her to the regional medical center at Mbarara for anti-venom treatment. She may lose her arm, but she’ll most likely survive this usually lethal experience.
My next patient arrived in advanced labor and I delivered a healthy girl. It was a very rewarding experience with an excellent outcome — no lacerations or complications, but very messy as we have no drapes or cloths. She gave birth on the tent floor in a pool of blood and amniotic fluid. My pants are now soaking in soap and water! We used surgical tape as an improvised umbilical cord tie.
The other patients started getting tired, angry and frustrated having to wait while we took care of these emergencies and many others. Fortunately, we were able to establish order.
Then my little eight-month-old burn patient who had been near death returned dehydrated from vomiting and diarrhea. It took us an hour to start her IV, but she improved after receiving fluids. Our last surgical patient was a three-year-old who injured his left foot in bike spokes. He literally ripped through his entire heel pad, exposing the bone and Achilles tendon. Fortunately, the bone and tendons are intact. It was a long repair — about four inches — but everything came together surgically, and we sent him home in a splint.

Today’s kicker: four children came to the clinic alone. The oldest is a 13-year-old girl who is caring for her three younger siblings. The youngest is just three, and they are living alone in a makeshift shelter. They fled Congo in November. Their father is either dead or stayed behind and their mother died in childbirth last month. They have no food and have survived because an adjacent family with four children of their own has been feeding them from their rations.
We arranged for a children’s protective service worker to come and check out the situation today. My heart was so touched. I so wanted to scoop them up and bring them home with me. They are so sweet and precious, and the oldest girl is a wonderful “mom.”
I couldn’t believe how tired we all were when we packed up at 7 pm. We saw 165 patients but seemed like twice that. Such is a day in the Nakivale refugee settlement. The camp is now at 40,000 residents and nearing capacity. Thankfully, they are digging a garbage pit for medical waste. The staff have tried burning our used equipment, but kids find the leftovers. Empty plastic water bottles are considered a prize! Burying waste is a much better solution.
We hope to have a water tank installed too as water shortages continue. Plans have developed for building a waiting area, a teaching room and additional exam area. Thankfully, we had a safe ride home. There are so many road accidents here. I collapsed in bed after dinner at 10 pm.
January 30
We began our day with a visit to Mbarara Regional Medical Center hospital to check on our three-year-old patient with a snakebite. She is still alive and gave us a weak smile, but her arm is not looking good. She’ll probably need a partial arm amputation. We prayed for this little girl — who is alive but for the grace of God.
We had 160 patients today and our work was very efficient because we had fewer emergencies. Our final patient came in with severe abdominal pain, so we took the opportunity to mentor staff about the importance of pelvic exams.
The staff honored us this evening with a feast of roasted goat…. We enjoyed speeches expressing their appreciation of our work and for God’s provision. We closed this magical evening with songs of praise and a prayer. We returned home late and will be back to work tomorrow.
Wishing you all a wonderful weekend. We will be home soon.
Report by Randall Jacobs, MD, from Juru, Uganda
In December, 2008, Medical Teams International (MTI) entered into a Memorandum of Understanding with UNHCR, GTZ, Office of the Prime Minister, Ministry of Health, and ICRC, to provide comprehensive health services to Juru ‘B’ sector with an unserved population estimate of 27,000. Critical needs: safe and adequate water supply, sanitation, food, acute medical care for malaria, pneumonia, sepsis, diarrhea, dehydration, malnutrition, antenatal care and midwifery services, HIV testing and counseling, immunizations. Pregnant women and children are most at risk. In mid December the first mobile medical clinic began serving the population at Kabahinda. In early January, a more permanent shelter was constructed and opened at the Juru ‘B’ site, 13 km from the main UNHCR base and health facility.
Mission: to reduce morbidity and mortality of Congolese refugees living in the Juru refugee camp and associated Nakivale settlement
MTI is providing a fully equipped and staffed semi-permanent medical facility at Juru ‘B’ providing medical and health services, including treatment of acute and critical pediatric and medical illnesses, minor surgery, antenatal care twice weekly, obstetrical assessments and referral, HIV testing and counseling, partnering with MOH for a biweekly immunization day, and referral with transportation to referral health centers (Nakivale health center and Mbarara University Regional Referral Health Center). Expanded services will include health promotion and education, distribution of insecticide treated mosquito nets, training of community health workers, monitoring-assessment-response to any disease outbreaks, and psychological services to refugees.
During the period January 7 to February 6, over 4000 patients were evaluated and treated, with no deaths reported.
Clinic resources
Staff: clinical officer, 2 comprehensive nurses, 2 registered nurses, 2 nursing assistants, 2 drivers, 7 interpreters (1 is a nursing assistant), 2 MTI volunteers
Facility: 6 room pole building with plastic tarp sheeting; 1 free standing tent
Vehicles: 1 ambulance, 1 double cab pickup
Pharmacy: generally well stocked for acute medical needs, no chronic disease medications, no TB meds
Minor surgery/parenteral fluids/meds: suture and instruments, IV supplies, parenteral drugs, and fluids; pediatric NG tubes, drapes and expanded suture selection needed
Ortho: splinting materials needed
GYN: speculums and light source needed
Testing: UA dip, urine preg tests, rapid HIV, fingerstick blood glucose, RDT for malaria, hemoglobinometer needed
Clinic days: Monday – Saturday, 150 – 300 patients per day
Related Links
- Medical Teams International
- Angels in Medicine: Medical Teams International and the Mobile Dental Program
