By Hannah McConnell, RN, BSN

Sabrina Richardson, a nurse and now also a missionary, has decided to dedicate her time to working with iReachAfrica. This ministry works in Mozambique and provides assistance to adults and children with healthcare, nutrition, education, and leadership training.

Prior to this, Sabrina spent several years as a registered nurse on an inpatient medical unit at Rady Children’s Hospital in San Diego. Working alongside children and families has always been her interest. On the medical unit, Sabrina worked with children with physical or intellectual disabilities, small children struggling with enteral feeding, and children with respiratory illness.
From the beginning of her education, she always had a desire to participate in medical missions. So, when Tracy Evans, a physician assistant and founding director of iReachAfria, came to speak at Sabrina’s church in San Diego and stated that they needed a nurse to fill a clinic position in a village in Mozambique, Sabrina felt a tug to say “yes.”
Since COVID, the clinic had been functioning as a food distribution center, as local Mozambicans were handing out milk to those who needed it.

Sabrina felt that timing in her life lined up to allow her to take this opportunity. Sabrina said, “six months before or six months after meeting Tracy, I could have given you a list of reasons why this would not work out,” but the timing now was just right. Sabrina felt that even her childhood of playing outside and being around bugs and snakes prepared her in a unique way to feel comfortable in various environments. Sabrina said that her education at Point Loma Nazarene University also prepared her for this, as she learned how to approach healthcare in a holistic sense. She stated that she feels secure “in this role, in this place, for this time.”
The clinic also has two Mozambican nurses and another American nurse. They fill the special role of a nurse with the opportunity to educate patients, ask thorough questions, and use a holistic approach.
Mozambique
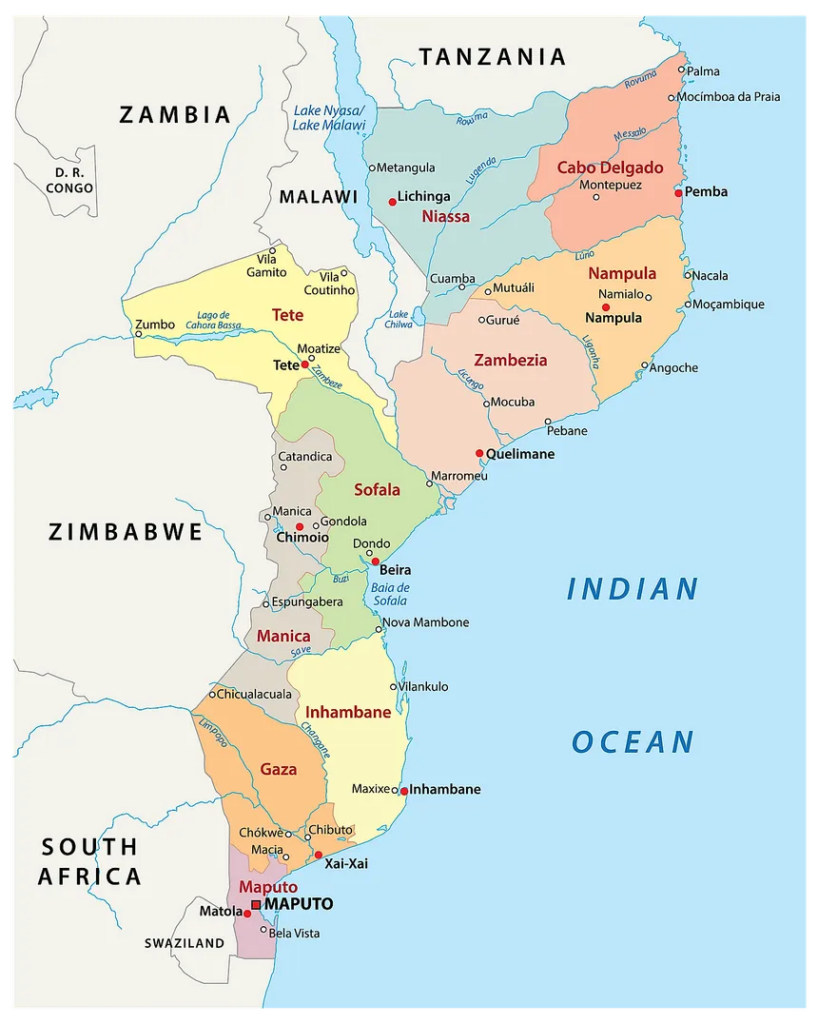
Mozambique is a country located in southeastern Africa, bordered by the Indian Ocean to the east. Portuguese is the language most widely spoken, although it is only spoken by half of the country. There are many local dialects that vary by region, Ciwute being the language spoken in the region where Sabrina works. However this language is not an officially written language.
Mozambique is one of the poorest countries in the world, ranked 181 out of 189 on the human development index. The poverty rate is 62.8% of the 33 million residents. Fewer than half of children complete primary school. The United States Agency for International Development states that there are “three doctors for every 100,000 people and more than one in ten Mozambican adults have HIV/AIDS.”
Clinic Overview

More than twenty five years ago, iReachAfrica was started because there was no access to infant and baby formula in Mozambique. The organization serves children, and in turn, their mothers as well. Supplementation is necessary in Mozambique: breastmilk is not always readily available. Sabrina shared that “death is such a typical part of life here,” so when mothers are sick in the hospital or when a mother passes away, there is no nourishment for the babies. Without access to breastmilk or infant and baby formula, caretakers put together a mixture of water, sugar, and cornmeal for the baby. This mixture as the sole source of food can lead to malnourishment. As a healthier alternative, the clinic provides powdered milk, or corn cereal with extra vitamins. The clinic also supports breastfeeding mothers and helps to supplement with food as needed.
Patients come to the clinic on foot or, if they are able, they ride with a “chapa” to the “milk stop.” A chapa is a collection of mini buses that is used for road travel. However, not everybody has access to this form of transportation. There is one family in particular that lives so far from the clinic and deep into the bush that they wake up in the morning and start walking, about four hours, in order to arrive at the clinic. Unfortunately, when the mother and child arrive, the child is unable to participate in the therapy because she is hungry and tired from the long journey. The clinic is working on a model to support this family and others in similar situations to be able to reap the resources they can offer. Despite these roadblocks, Sabrina states that these families do “not complain about anything.”

For appointments for therapies, families will come to the clinic on the date that they are scheduled. It is a challenge to keep track of time due to the long commutes from home, lack of electricity and other responsibilities that may be unforeseen.
Children are visited at the clinic until they are a year and a half. During this time, the clinic also provides education on the need for protein and reinforces their support of the family. The discharge process is quite long to ensure that the child’s guardian has the education and resources to continue to sustain their child. Unfortunately, some children have returned very malnourished, with large bellies and edema in their feet and hands due to the lack of protein. The clinic therefore continues to adapt their processes and explores “how can we be sure that the children in this program are going to be successful after discharge?”
Special Needs Program
The clinic also offers a special needs program. There is a range from high functioning to low functioning disabilities in these children, with either physical or intellectual disabilities. There are many kids in their late teens that could be seen, but since these kids are too large to be carried on the backs of their mothers or caregivers, they are not able to visit the clinic. Mothers or caregivers come to collect food and resources to bring back to their children at home. Sabrina understood from her previous work experience the special role that families play in the life of a child with special needs and how important the resources are for them. In addition to supplemental formula, they have begun to provide play therapy for the children.

Sabrina shared that there is accusation and shame that surrounds having a child with special needs. It is thought to be a curse or something that the mother did at birth to be punished with a special needs child. To address this, the clinic has formed a group of mothers and kids with special needs. Two mothers at the clinic told Sabrina, “We feel like family now.” The mothers have found support in each other, sharing different techniques to help their children, building friendships together.
Roadblocks and Wins

There have been many roadblocks throughout the process that Sabrina’s team pushes to overcome. For example, seizure medications have been a challenge to have prescribed, because historically they are only prescribed for a number of days, rather than for months or years. Now, the clinic writes notes, stamped and signed, in hopes that they will aid in the prescription of the proper medication with monthly refills. Recently, Sabrina shared a story about a mother who returned to the clinic with an entire month’s supply of the medication, with a receipt for monthly refills. The daughter of this woman, a four-year-old, began to babble “mama” the day that she started taking the medication. When Sabrina learned this, she felt rewarded. To see that ones efforts make a difference is a gift.
Another challenge Sabrina faces is the lack of access to many resources. For example, feeding tubes would provide nourishment for kids who are unable to take food by mouth; however, this is not a procedure that they do. In addition, Sabrina also spends her time with grieving mothers whose children have passed away. Follow-up care has also proved to be a challenge, which makes it difficult for kids to continue to receive the care that they need.
Day-to-Day Life: Food, Transportation

Sabrina described the land this way: “the dirt is so red, the sky is so blue, and the grass is so green.” Her way of life has changed tremendously since she arrived in Mozambique, through her diet, surroundings, and culture. She said that the staple food in this region is corn, which is milled and ground by hand, then mixed with water to create a paste. It is called xima, pronounced “shima,” and is eaten with stewed greens or beans. Meat is saved for special occasions or holidays. They grow peanuts, which are available in abundance. Most of the food is made from scratch, such as ricotta cheese.
Most people get around by foot, although there is also access to chapas mentioned previously. Sabrina is taking lessons in both Portuguese, and in the local dialect in order to improve communication with the people around her.
Conclusion

Sabrina originally made a commitment to work in Mozambique for two years, but a year and a half in, she is sure that she will stay for much longer. After six months of struggling to communicate well and learn the language, she feels that many of the ideas that they have implemented are just beginning to blossom. The clinic is functioning well, the Mozambican nurses are being educated, and the systems have been changed many times and are now running much smoother. She would love to stay and see it through for longer.
Sabrina believes that things will continue to improve at the clinic to better support those in surrounding areas. They are working hard to establish relationships with the local hospital in order to build trust and work together to improve the systems. Over the last couple of years, Sabrina has observed differences in the relationship that the clinic has with the local hospital. She has been able to observe, for example, a patient receiving HIV education, and was very impressed with the testing and support that the hospital provided. This is one of the many things that has continued to encourage the team to keep building. The relationships with local hospital workers are allowing for more efficient and thorough care and proper education, and respect for one another. She has built relationships with several providers at the hospital, who are struggling, as their patients are suffering, due to the minimal resources. Sabrina said that they are “such good people doing the best with the resources they have.”
About the Author

Hannah McConnell is a registered nurse and freelance writer. In her free time, you can find her swimming in the ocean or trying a new recipe in the kitchen. You can reach her at hannmcconnell@gmail.com or on her LinkedIn page.
