First published on August 3, 2023 by UIC Today. Credit: Carlos Sadovi, UIC Today.

As more migrants were making their way from the border to the Chicago area, a group of University of Illinois Chicago medical students formed the Mobile Migrant Health Team to provide care for them.
Since the first week of May, more than 3,000 migrants have received medical attention from the UIC student-driven group, which has volunteered at nearly a dozen Chicago police stations where migrants are being sheltered.
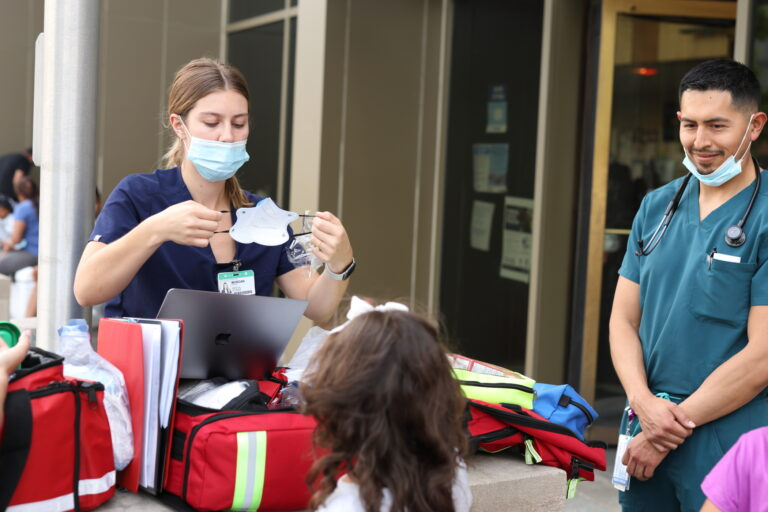
Recently, the Mobile Migrant Health Team visited the 12th District, near Chicago’s Pilsen neighborhood, and reviewed medical supplies, including over-the-counter medications, forms, masks and other materials.
On this day, first-year medical student Sara Izquierdo, was joined by fourth-year medical students Sara Cooper, Morgan Pooler and Leena Jehad Abbas, along with Dr. Alex Lucas, a second-year resident at Advocate Christ Medical Center, and Dr. Beth Payment, a family practitioner from West Suburban Medical Center.
The team, which Izquierdo began with the assistance of Dr. Evelyn Figueroa, a family medicine doctor at UI Health, has grown to include 80 active volunteers, including UIC medical students, physician assistants, nurses and doctors from other hospitals.
The teams of bilingual students make several weekly visits to police districts throughout the city and are overseen by physicians like Lucas and Payment, who are licensed to provide treatment.
“It’s incredible — they give us such good attention, and it’s not the first time they’ve helped us. They’ve given me some medication for my child’s allergies,” said a 29-year-old woman who has been sleeping at the 12th District station for more than a month since arriving in Chicago with her young children after leaving Colombia.
“We had to leave in the middle of the night when a group of bad men showed up and threatened us,” she said.
Izquierdo, who received her bachelor’s degree and master’s in public health from UIC, said many of the people on the team are immigrants themselves or, like herself, from families of immigrants.
“There is a lot of identification with the population we are serving,” Izquierdo said. “It feels like something that needs to be done because if we’re not doing it, no one is.”
Meeting people where they are
During the pandemic, Izquierdo had been involved in community organizing and engagement with neighborhood vaccination campaigns and grassroots organizations. Then, an alderwoman asked her for help.
“She basically said, ‘Hey we’re having a bit of a health crisis at the police stations right now with the recently arrived migrants — is there anything we could organize or do?’” Izquierdo said.
Izquierdo took what she learned from being part of Chicago Street Medicine, an initiative that began in 2016 with several UIC students and a UIC resident physician providing medical attention to people experiencing homelessness.
“I really like the model of bringing medical care in a mobile way to meet people where they’re at,” Izquierdo said.
After reaching out to others about how to tailor what she had learned through her work with Chicago Street Medicine, Izquierdo met Figueroa, who has been on the UIC faculty for 18 years. Figueroa offered to help lead the initiative.

Figueroa joined Izquierdo and other students who came up with the plan to have bilingual medical students triage migrant patients, write down their medical histories and present them to attending physicians.
“Since then, every few runs if something works better or if the police station has changed how they want us to do things, we’ve been very adaptable, and it’s been very effective,” Izquierdo said.
Figueroa said that over the years she has been involved in street-based medicine and has treated people living in shelters. She has a nonprofit organization separate from UIC that serves as the fiduciary sponsor for the Mobile Migrant Health Team. She helped structure the initiative to meet compliance issues and best practices.
“Sara has great instincts, so it was just me putting little, tiny guardrails,” Figueroa said.
Gathering health histories
At the stations, they speak to the migrants about urgent or emerging health-related issues they may be experiencing. They provide treatment on-site and provide follow-up opportunities and appointments for issues such as long-term prenatal care.
Because the medical students have not received their licenses, they can provide general medical advice but cannot treat patients themselves, Figueroa said. They aim to have a team of five to 10 people and never go without a licensed physician.
The students gather health histories and provide over-the-counter medication with English and Spanish labels to treat things such as colds and other minor health issues.

At the 12th District, a 42-year-old woman spoke with Jehad Abbas, a fourth-year UIC medical student, and Lucas about the foot pain she was experiencing. Jehad Abbas listened as the woman described a stinging pain. Lucas listened as Jehad Abbas spoke in Spanish, then asked his own questions, also in Spanish. After Jehad Abbas presented the woman’s ailments to Lucas, he agreed with her assessment and provided medication.
“I come from the Latino community and in the hospital, I mainly serve the Latino community, so doing this now in the streets is really rewarding,” Jehad Abbas said.
Figueroa said that about 80% of what they do are “pretty bread and butter” health issues. But when there are more pressing issues, they send the patient to the nearest emergency room. They provide documentation that the person is experiencing homelessness. Izquierdo and the other students help patients with expenses through fundraising efforts and Figueroa’s nonprofit organization.
In addition, the Mobile Migrant Health Team works to find primary care homes where long-term health issues, such as diabetes, high blood pressure, pregnancy, asthma and lupus, can be treated.
Developing innovative ways of delivering care
“The police stations became this no man’s land in a lot of different ways, and it was really individuals who stepped up to help,” Figueroa said. “I think it’s just amazing when you can work with these young minds who just don’t accept no as an answer, want health equity, and push to develop innovative ways of bringing health care in a dignified and humanistic fashion.”
In addition to the mobile team, since September, UIC doctors specializing in pediatric patients have been working with the National Youth Advocate Program, which provides services to unaccompanied children and tries to find placement for them with foster families.

The partnership was led by Dr. Sarah Messmer, an internal medicine and pediatric specialist at UI Health, and Dr. Lauren Williams, an internal medicine and pediatric specialist at UI Health Mile Square Health Center in Cicero, where she is also the site medical director.
“We have committed to providing their initial medical exams, which are required within 48 hours of their arrival and then any other medical and primary care needs that they have,” Messmer said.
The physicians team up with a coordinator from the National Youth Advocate Program to provide the children’s required initial health exam. The UIC physicians also follow up with additional care the children may require. The youngest child they’ve evaluated is 2 years old.
Since last September, the physicians in the Child and Youth Center at UI Health in Chicago have conducted about 75 evaluations. About 30 evaluations have been completed at Mile Square in Cicero since they began working with NYAP in March.
The work has been led by pediatric care residents and is structured so that the residents are primarily evaluating the children while an attending doctor oversees their efforts. Three residents are on the global health track and are training others to conduct the evaluations.
Helping to ease fears
Among the issues they might focus on is trauma-informed care. This is because many of the migrant children have arrived after traveling by land across several countries, sometimes alone at young ages.
“A lot of these children have had traumatic journeys from wherever they are coming from,” Messmer said. “They’ve been through so much. I think a big part of what our residents really focused on learning and getting more experience in is how to care for these children.”
Williams said her nursing staff has been amazing and has collected toys to provide to the children to help ease their fears.
“Each NYAP kid gets a toy, whether it is a coloring book or a doll or even games so that when they come here, their first introduction to the U.S. is something that is a pleasurable one even though we are giving them shots and taking blood,” Williams said.

Coordinators with NYAP are in contact with UIC officials to schedule appointments and inform them of recent arrivals of children. NYAP is alerted of unaccompanied minors, and they take custody of the children and coordinate with medical officials to get the required examinations and vaccinations.
The children they see receive temporary housing with a foster family and may be reunited with a parent or family member who had been living in the United States before the child arrived.
“These kids have been through so much, the least we can do is try to make their experience coming to the United States as least traumatic as possible and support them as they try to reunify with a family member,” Messmer said. “This falls very clearly within the mission of UIC, UI Health and Mile Square to provide services for our community, and these children are part of our community.”
Williams said the ability to serve the community has been meaningful to her and the staff at Mile Square.
“Especially at Mile Square, our mission is that we don’t turn patients away, and we also take care of those who don’t have the opportunity or the resources to take care of themselves,” Williams said. “This speaks to the heart of it. Being involved keeps us grounded and reminds us that every day we are still doing great things, and we are able to do little things for those who need us.”
